With today’s aging population, eye problems such as cataracts, macular degeneration, retinitis pigmentosa and glaucoma are all becoming more common. Researchers around the world are developing new and enhanced light-based technologies that are enabling ophthalmologists to make earlier and more accurate diagnoses, and provide treatment that ultimately will slow or prevent blindness. A group in California is combining optical coherence tomography (OCT) with adaptive optics. A team in New Zealand is studying a detection technology borrowed from quantum optics. And the NIH is backing research on a new approach to trabeculoplasty for glaucoma patients.
OCT with adaptive optics detects deformations in rods and cones
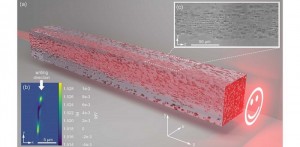
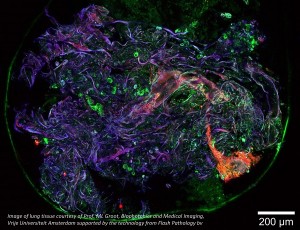
A team from the University of California Davis Eye Center is using a new optical coherence tomography (OCT) tool to detect the function of rods and cones in the eye, and it may one day detect macular degeneration much earlier. The instrument measured tiny light-evoked deformations for the first time in individual rods and cones in a living human eye.
"Our instrument offers a unique way to study retinal disease at the cellular level," said research team leader Ravi Jonnal
The team was able to measure how individual rods and cones respond to light by using a high-speed OCT system capable of detecting slight swelling in the outer segments of the photoreceptors that occurs as a side effect of phototransduction. This is done by capturing specialized OCT images simultaneously with scanning light ophthalmoscope images, enabling it to pinpoint the location and type of photoreceptors captured in a series of hundreds of 3D OCT images. Recently, full-field OCT has been used to visualize the light-evoked deformation of larger peripheral cones. Because the light-evoked deformation of photoreceptors can be very fast, the new system incorporates a high-speed Fourier-domain mode-locked laser that enables fast imaging and can scan 16 times faster than commercially available lasers used for swept source OCT.
To capture the highest resolution images possible, the researchers incorporated adaptive optics technology that measure the eye's aberrations and corrects them in real time. Even with adaptive optics, rod photoreceptors are too small to be imaged due to the system's 1-micron-wavelength light source. To overcome this problem, the researchers added a scanning light ophthalmoscope imaging channel that uses a wavelength that is less than 1 micron to increase the imaging resolution. This allowed differentiation of rods and cones in co-registered OCT images. The researchers measured the deformations of rods and cones in response to light of varying intensity in living human eyes, and they found that the responses of the cells increased as the light intensity increased until saturation occurred, consistent with phototransduction.
The work is part of an emerging international field of research that aims to develop methods to fully capture the function of the retinal neural circuit of living people.
Read more in “OCT-based Technique Captures Subtle Details of Photoreceptor Function” .
OCT with less light required
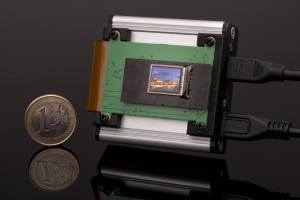
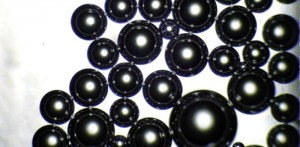
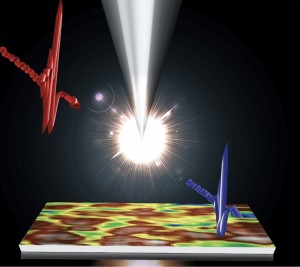
In New Zealand, researchers are using a detection technology borrowed from quantum optics to perform OCT with much lower light power than previously possible. The team replaced standard OCT detectors with superconducting single-photon detectors (SSPDs), a technology used in quantum optics to distinguish individual photons. This setup allowed them to achieve good image quality with power levels up to 1 million times lower than those currently used in OCT instruments.
“For clinical applications, being able to perform OCT with low light power is crucial because safety standards limit the light intensity levels that can be used,” said research team leader Sylwia Kolenderska from The University of Auckland. “In some cases, these power levels are not high enough to achieve good image quality.”
Incorporating SSPDs into a standard OCT system required some changes to the typical optical setup. Modern OCT instruments work by discerning the colors, or wavelengths, of light reflected from an object. This wavelength discrimination can be performed by using a single pixel detector while the light source produces one wavelength at a time, or it can be done with a diffraction grating that splits the light into different wavelengths like a prism and a camera that detects these wavelengths.
The researchers used a fiber instead of a grating to separate different colors, which each travel at different speeds down the fiber. At the fiber’s output end, they used the SSPD to capture the different colors as they arrive at different times. This allowed the light spectrum to be acquired for reconstructing OCT images.
“In the future, if single-photon detection technology could be made much smaller and less expensive, a line of portable diagnostic machines based on light-based imaging might be created for safe self-diagnosis purposes in the comfort of one’s home,” said Kolenderska.
Read “Quantum Inspired Approach Dramatically Lowers Light Power Needed for OCT” .
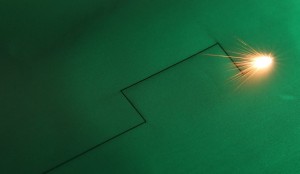
A new approach to SLT laser treatment for glaucoma
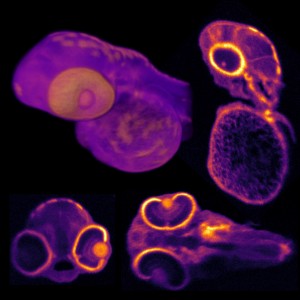
Glaucoma is an eye disease where the intraocular pressure is elevated and, if left unchecked, can cause loss of peripheral vision or blindness. It is often manageable by having the patient use daily eye drops; however, because eye drops are an inconvenience, are easy to forget, and can come with side effects, this team of researchers from the University of Pittsburgh and West Virginia University are studying how selective laser trabeculoplasty (SLT) can better treat glaucoma
Like eye drops, SLT also treats glaucoma by lowering eye pressure, and it has been used successfully for many years. In this study they are comparing traditional SLT to low-energy SLT, which may have the advantage of being able to be applied more often. If successful, glaucoma patients may be able to do away with eye drops altogether, and opt instead for annual SLT treatment.
“Our hope is that a brief low-energy laser procedure performed in the office once a year will effectively lower eye pressure without the hassle, expense, and side effects of daily medical therapy,” said the study’s principal investigator Dr. Tony Realini, professor of ophthalmology and glaucoma specialist at WVU.
Read “Low-Energy Laser Treatment Study Supported by National Eye Institute” .
Written by Anne Fischer, Editorial Director, Novus Light Technologies Today

























 Back to Features
Back to Features