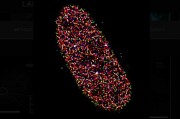
Lung cancer is most common cancer in men and the 2nd most common cancer in women according to World Cancer Research Fund International. Lung cancer is the leading cause of cancer death overall and among both men and women, according to the American Lung Association. Lung cancer typically is not obvious, showing few if any signs and symptoms in its earliest stages, which is why early detection is important. Lung cancer screening involves using imaging to detect cancer, and then a diagnosis is made by removing lung cells from the patient, and examining the cells in a lab.
Types of imaging used to detect cancer include chest x-ray, computed tomography (CT) scan, magnetic resonance imaging (MRI), positron emission tomography (PET).
A chest x-ray is often the first test that a doctor orders to look for any abnormal areas in the lungs. If something seems abnormal, further scans may be ordered.
- The CT scan uses x-rays to make detailed cross-sectional images of the body. The scanner takes many more pictures than a standard x-ray, and a computer combines them to show a cross section of the lungs. The advantage of a CT scan over an x-ray is that the images can show the size, shape, and position of tumors and also spot enlarged lymph nodes and other organs, which that might indicate that the cancer has spread.
- The MRI is similar to a CT scan, but it uses radio waves and strong magnets instead of x-rays. MRI scans are most often used to look for possible spread of lung cancer to the brain or spinal cord.
- The PET scan uses a radioactive form of sugar (known as FDG), which is injected into the blood and collects mainly in cancer cells. Often a PET scan is combined with a CT scan using a special machine that can do both at the same time because the CT scan provides a detailed picture, while the PT scan shows areas of higher radioactivity. If your doctor thinks the cancer might have spread but doesn’t know where.
Calling for improvements
While these forms of imaging have been used for many year, cameras and imaging equipment continues to advance and scientists are improving procedures. The International Atomic Energy Agency (IAEA), in cooperation with experts from seven cancer care organizations, developed the paper calling for improvements in medical imaging and nuclear medicine infrastructure to improve outcomes for lung cancer patients throughout the world. The paper “Toward Improved Outcomes for Patients With Lung Cancer Globally: The Essential Role of Radiology and Nuclear Medicine” was published recently in the Journal of Clinical Oncology (JCO).
The scientists noted gaps in diagnostics and treatment in various countries, as noted in the IAEA Medical Imaging and Nuclear Medicine Global Resources Database (IMAGINE), which reveals inequities in diagnostic capacities in different countries. For example, one CT scanner serves an average of 25,000 people in high-income countries compared with 1.7 million people in low-income countries. After a diagnosis, the patient must be treated—yet cancer treatment services are scarce in low-income countries (90% availability in high-income countries versus 30% in low-income).
The study brings together data and research covering the entire global lung cancer landscape, pointing out gaps in diagnostics and treatment therapies worldwide. What is key to treating cancer is early diagnostics, and that is true anywhere in the world.
“Early-stage lung cancer can be treated, but most patients, especially in low- and middle-income countries where there is a lack of access to both diagnostics and therapies, only come for diagnosis when they are already in advanced stages,” said Miriam Mikhail, a Diagnostic Radiologist at the IAEA and one of the authors of the article. In global public health strategies for lung cancer, the focus has been upon removing known causes; for example, tobacco, radon and asbestos. Mikhail said that a concurrent emphasis on early diagnosis could lead to life-prolonging interventions and life-enhancing palliative measures, including impactful low-dose CT screening of those at high-risk of developing lung cancer.
“Improved population-based outcomes are attainable,” she said. “With this paper, we hope to galvanize high-level strategic dialogues on how medical imaging infrastructure improvement is a key puzzle piece to fight lung cancer.”
Where lung cancer diagnostics and treatment vary in countries around the globe, there is a disproportionate number of people who die prematurely or suffer needlessly because their lung cancer was not detected early enough for effective treatment. The authors of the study sought to show how global research has proven that by using appropriate imaging methods to inform the treatment selection ultimately leads to measurably better results for patients and the country, in the mid and long term.
IAEA experts worked with counterparts from the Abramson Cancer Center of the University of Pennsylvania, the University Hospital Zurich, the European Society for Medical Oncology, the European Association of Nuclear Medicine, the Tata Memorial Centre, the Memorial Sloan Kettering Cancer Center and the MD Anderson Cancer Center to develop the study.
Paper: DOI: 10.1200/GO.21.00100 JCO Global Oncology no. 8 (2022) e2100100. Published online June 1, 2022.
Written by Anne Fischer, Editorial Director, Novus Light Technologies Today

















 Back to Features
Back to Features