With the current pandemic, everyone is trying to do their very best to contribute to global containment and prevention efforts. This situation creates a need to monitor and control access to febrile (fevered) individuals in what we have come to know as “essential” commercial and public-facing services. This concern for detecting fever is not new. In the east, fever detection was used with the 2002-2004 SARS outbreak, and is now essential with the current COVID-19 pandemic.
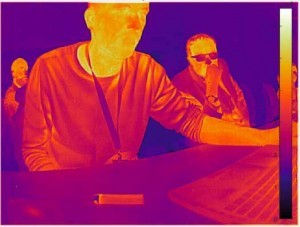
Many articles were published on fever detection after the SARS outbreak, generally focusing on alternative and mostly non-contact methods (to avoid the spread of the virus). The most mainstream methods are handheld thermal thermometers and thermal cameras. According to a cursory review of the relevant literature on the subject, thermal cameras seem to be much more reliable and accurate then the handheld thermal thermometers, but only by following the guidelines around how and where to perform the measurements.
In fact, literature on the use of thermal imager devices for fever detection dates back to 1985 when Walter T. Hughes published “Detection of Fever with Infrared Thermometry: A Feasibility Study” in the Journal of infectious Disease. In this article, he states: “The eye and E spot [areas below the ear lobes] provided the most accurate readings. Infrared measurements of the right eye identified 57 (95%) of 60 febrile and 72 (90%) of 80 afebrile patients correctly. Overall, 92% of all patients were correctly categorized by use of the infrared thermometer at this site. We conclude that this approach is feasible and, with further technical developments, may be applicable for routine clinical use.”
Early fever detection methods
In 1985, Doctor Hughes was using a pyrometer to perform the tests, which is an early version of the devices used in the handheld spot meter; these are commonly used in attempts to detect fever in a line of people. There is a particularly interesting part in this publication where the author elaborates on the technical limitations of the thermal imaging technology of that time:
“Three technical improvements of the instrument can be easily accomplished. Perhaps most important would be the incorporation of a microprocessor to calculate a mean value for multiple readings from the target site. With the instrument used in our study, the operator was required to mentally estimate the mean reading from rather rapid fluctuations on the digital display. Although the range of these readings was greater than 1 degree C, a microprocessor with a memory would provide more precise measurements. … A second improvement would be a visible indicator to show the target site being recorded. With the instrument used in our study one was required to hold-the probe aimed at the target and simultaneously observe the digital readout.”[ii]
These recommendations were both eventually developed for spot meter (time averaging and laser pointer to mark the measurement spot). However, these spot meters still suffered from the large area of the face being measured, covering cooler and warmer spots of the face unless the unit is held very close to the person´s eye (which might be impractical in some situations). Also, I have noticed in some videos that the person using the spot meter tool often test the forehead of subjects without asking them to move their hair out of the way. This is likely a large loss of accuracy, since the human hair isn´t technically alive and its emissivity is so much lower than the human skin, it would return a generally lower temperature then the person´s body temperature. For these measurements to work, it is crucial to measure the person´s temperature in the right spot. For this purpose, thermal imagers are superior to thermal spot meters since they systematically measure the whole scene and then only the desired information can be extracted from the image.
Best practices for temperature measurement
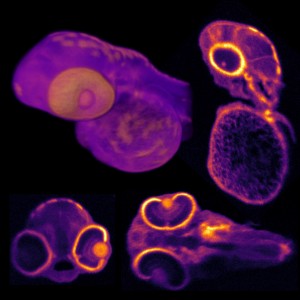
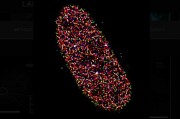
According to many different clinical studies[iii],[iv],[v],[vi] along with a thorough literature review and published standard by ISO[vii], IEC[viii] and recommendations from the CDC[ix], the best place to measure a person´s body temperature for the purpose of fever detection is the lacrimal caruncle area of the eye (the inner part closest to the nose where your tear ducts are) or the ear hole. Temperatures can also be measured and averaged over large areas of the face but the actual temperature returned by such a measurement might vary according to the heart rate of subjects or from person-to-person based on blood pressure and variations in the heat distribution in the face (heavy sweating for example).
So the best practice for such screening is to have the person face the camera in a mug-shot like infrared image.
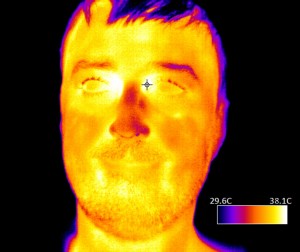
Then a measurement can be taken in close proximity to the individual´s lacrimal caruncle area. The thermal camera can convert the signal of each pixel to receive absolute temperature measurements.
It is also much more reliable and precise for cameras to compare relative temperature increases than to attempt to relate to the absolute temperature of the objects in the scene. So, it is recommended to include in such systems some sort of reference where the scene will include a known temperature reference (usually a black body radiator). This is particularly important in the case of fever detection since the threshold between healthy and feverish is very slim and close to the systems absolute accuracy.
Fever detection during the COVID-19 pandemic
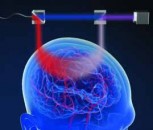
Considering the growing pandemic crisis, many organizations are rethinking how we monitor entry into public buildings "such as hospitals, food or medical equipment production facilities, or other essential workplaces " during the outbreak. A fever is a symptom of COVID-19 and many other viral infections, and thus can be used as a screening mechanism to help identify potentially infected individuals.
Today, Walmart and Amazon are checking employee temperatures with handheld thermometers, but that limits how fast workers can be checked, and the people using the scanners must be close near the people they are checking, which increases their risk of infection.[x] With a thermal camera, an initial scan can be done automatically as a line of people file into a building. If it is identified that someone has a fever, that person can be checked again by a medical professional with a handheld thermometer.
Of course, fever detection is just one tool to slow the transmission of the virus. People with COVID-19 can be asymptomatic or may not yet have a fever. Or, they may have taken medications to reduce a fever. However, fever detection with thermal cameras does provide additional data that was previously unavailable in an easy and streamlined way. Going forward, businesses are more likely to implement thermal camera technology in a proactive manner, such as at airports or as part of a border control check. The promise of rapid, easy-to-use fever detection has caused a huge surge in demand for thermal cameras.
Take care of you and yours in these troubled times.
Written by Jean Brunelle, a product manager at Teledyne DALSA,
Endnotes:
Walter T. Hughes, Gayle G. Patterson, Delaine Thornton, Bonnie J. Williams,
Lennie Lott, and Richard Dodge - THE JOURNAL OF INFECTIOUS DISEASES • VOL. 152, NO.2· AUGUST 1985
[ii] Hughes, ibid.
[iii] Sun G, Matsui T, Kirimoto T, Yao Y, Abe S. Applications of infrared thermography for noncontact and noninvasive mass screening of febrile international travelers at airport quarantine stations. In: Ng EYK, Etehadtavakol M, editors. Application of Infrared to Biomedical Sciences. Singapore: Springer; 2017. p. 347"58.
[iv] Ring F. Pandemic: thermography for fever screening of airport passengers. Thermology International. 2007;17(2):67.
[v] Cowling BJ, Lau LL, Wu P, Wong HW, Fang VJ, Riley S, et al. Entry screening to delay local transmission of 2009 pandemic influenza A (H1N1). BMC Infect Dis. 2010;10(1):1
[vi] Mercer JB, Ring EFJ. Fever screening and infrared thermal imaging: concerns and guidelines. Thermology International. 2009;19(3):67"9.
[vii] ISO. ISO TR 13154: Medical electrical equipment"Deployment, implementation and operational guidelines for identifying febrile humans using a screening thermograph. International Organization for Standardization; 2009.
[viii] IEC/ISO. IEC 80601-2-59: Particular requirements for the basic safety and essential performance of screening thermographs for human febrile temperature screening. Geneva, Switzerland: International Electrotechnical Commission (IEC) / International Organization for Standardization (ISO); 2017.
[ix] CDC. Non-Contact Temperature Measurement Devices: Considerations for Use in Port of Entry Screening Activitie. 2014.
[x] Nellis, Stephen. "As Fever Checks Become the Norm in Coronavirus Era, Demand for Thermal Cameras Soars." Reuters, Thomson Reuters, 9 Apr. 2020.
















 Back to Features
Back to Features