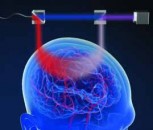
To test complex brain functions during neurosurgical procedures, surgeons must operate on awake, locally anesthetized patients. This allows surgeons to interact with them and test how their intervention affects brain function. However, opening the skull while the patient is awake is extremely stressful for them psychologically. A new robot-assisted and optically precisely monitored laser procedure developed by the Fraunhofer Institute for Laser Technology ILT in Aachen is set to enable gentle, vibration-free and virtually silent craniotomies while the patient is awake. The bone tissue of the skull is ablated using short-pulse laser radiation.
Many people shudder at the mere thought of having brain surgery while they are awake. Those affected are confronted with a frightening procedure: During a craniotomy – the opening of the skull – the bone material is removed using mechanical instruments that literally shake the patient. The noise and strong vibrations – perceived intensely – cause severe psychological stress. Awake operations are, therefore, usually carried out if only a small opening in the skull is required for the procedure, for example for deep brain stimulation in the case of severe movement disorders. Larger craniotomies, which are necessary for the removal of brain tumors, for example, are too stressful for awake patients.
If surgeons could interact with a patient during brain tumor removal, they would have an important control option during the process. Particularly when regions of the brain critical for speech and motor function are affected, surgical teams could test at any time whether the removal of tissue triggers functional deficits. Thanks to this control option, tumors, among other things, could be removed more radically without impairing brain function. In the long term, this could significantly improve the prognosis of affected patients. The situation is similar to the implantation of pacemakers for deep brain stimulation (DBS). In order to optimize how effective electrodes for brain stimulation are against severe shaking palsy caused by Parkinson's disease, for example, they must be positioned with high precision in the affected areas of the brain. "DBS is used very successfully today to treat shaking palsy. However, due to the stressful awake craniotomy, many patients still forgo the procedure, despite the success of this method," says Dr. Achim Lenenbach, head of the Laser Medical Technology and Biophotonics Department at Fraunhofer ILT.
Contactless surgery
To maximize the chances of success, medicine must give patients undergoing awake craniotomies psychological relief. Lenenbach and his team are developing an innovative, robot-assisted laser procedure for this purpose. The switch from mechanical instruments to laser technology is intended to make craniotomies virtually silent, vibration-free and gentle, so that awake neurosurgery can be performed much more frequently than before. The procedure is also intended to minimize the risk of meningeal injuries during craniotomy and improve the post-operative healing process by sensory control of the laser process.
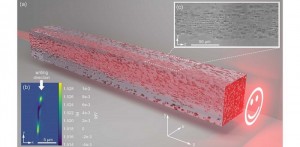
With this goal in mind, the team in the STELLA project is developing an efficient, safe and largely automated laser cutting process. The core component is a CO2 laser with 120 nanosecond (ns) short laser pulses. The short pulses ensure that no carbonization effects occur as a result of heat input at the cutting edges. This is because thermal damage to the bone tissue impedes the healing process. Since the exposure time is so short, the ns pulses remove the hard tissue without significantly heating the surrounding tissue. The new laser procedure leaves clean and thermally unaffected incision edges. However, efficiency is also important in everyday clinical practice. "We are currently achieving ablation rates of 1.6 cubic millimeters per second (mm³/s)," reports Lenenbach. For clinical applications, an efficient cutting process requires 2.5 mm³/s. To achieve this, a solid-state laser tailored to the bone cutting process is used.
Conversion to a solid-state laser developed at Fraunhofer ILT
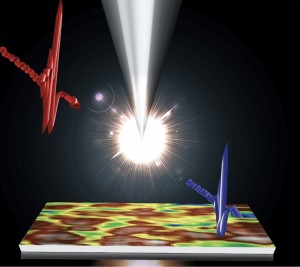
Previously, the CO2 laser beam was guided via an articulated mirror arm. However, in order to increase efficiency, reproducibility and flexibility, the Fraunhofer team has equipped the laser craniotome with a fiber-guided solid-state laser that emits 100 ns short laser pulses in the mid-infrared spectral range around 3 µm. "Light with this wavelength is absorbed very well by bone tissue, can be guided in a fiber and is, therefore, easier to combine with the robot than CO2 laser radiation," says the expert. The combination with the robotic arm could also pave the way for further medical applications. Among other things, this is interesting for spinal surgery, which is risky due to its proximity to the spinal cord. The sensor-controlled short-pulse laser process could minimize risks here.
Since the short-pulse laser source in demand for laser craniotome – with a wavelength of 3 µm and a pulse duration of 100 ns – is not commercially available, the Lasers and Optical Systems Department at Fraunhofer ILT is developing it together with industrial partners. This brings the targeted ablation rates within reach without causing thermal damage to the surrounding hard tissue.
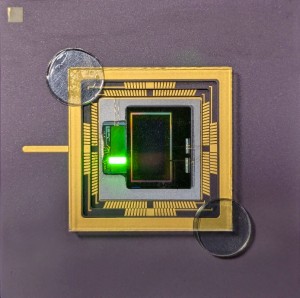
Sensory monitoring of the laser cutting process
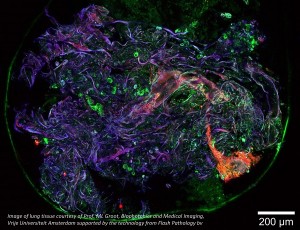
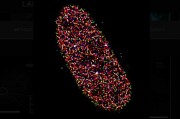
The laser cutting process is monitored by an OCT (optical coherence tomography) measurement system to ensure that the laser beam actually only removes bone tissue and that the underlying structures such as the meninges or spinal cord remain undamaged. An OCT measuring beam superimposed on the cutting beam determines the local cutting depth and residual thickness of the bone. The process stops immediately before the bone is cut. The remaining fine bone lamella can then be removed from the composite with little effort and without risk of injury. Since it precisely controls bone removal, the process ensures that the tissue under the skull or in the spinal canal is protected effectively. "To achieve this, software continuously evaluates the sensor signals, recorded synchronous to the process, and transmits the results to the real-time control of the laser surgical system," explains Lenenbach. The inline OCT sensor system also shows the surgeons how the removal of the bone tissue is progressing. Once the almost silent cutting process is complete, they can lift off the loosened skull cap to begin the neurosurgical procedure. The bone flap is then reinserted and quickly grows back together with the surrounding tissue thanks to the gentle laser cutting process.
Virtual system model
During the development process, a virtual system model of the laser craniotome enabled the team to investigate any technical disruptions in the craniotomy process and to virtually test the influence of individual system components without modifying the hardware. This allowed them to test alternative scanner models, perform the process with an automated stereotactic system or with a collaborative robot, and optimize the virtualized system very efficiently. "Virtualization has become a very important tool for us to design and test laser-based surgical systems and gradually bring them closer to clinical practice," concludes Lenenbach. Digital prototyping is an important tool for efficient development processes.
STELLA demonstrator at MEDICA 2024
Interested parties can find out more about the technology at the leading trade fair MEDICA in Düsseldorf from November 11 - 14, 2024. The Fraunhofer ILT team will be presenting the STELLA demonstrator at the joint Fraunhofer stand in Hall 3 Stand E74.

















 Back to News
Back to News